In Breast Cancer Care, Choose Wisely
Published: July 29, 2016l
By Helen Pass, MD, Director of Breast Surgery and Co-Director, Breast Center
The American Board of Internal Medicine Foundation started the Choosing Wisely campaign in 2012 to provide guidance and discourage the use of unnecessary medical interventions. They gradually partnered with national medical societies to provide specialty appropriate recommendations. Last month, the American Society of Breast Surgeons (ASBrS) published their breast specific recommendations.
Schedule a Mammogram
Get Same-Day Results During Business Hours
Call 203.276.PINK (7465)
Let’s review the 5 measures endorsed by the ASBrS and provide some perspective. It is important to recognize that these guidelines are merely guidelines and sometimes best medical care may deviate from these recommendations. Nevertheless, they are a very good starting point to initiate the conversation between you and your doctor and encourage the incorporation of best available evidence. We hope you find the following helpful when having a thorough conversation with your doctor:
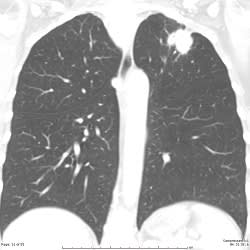
1. Don’t routinely order breast magnetic resonance imaging (MRI) in new breast cancer patients.
The key word in this sentence is "routinely." In medicine, it is generally not a good idea to either always or never do something since patients are individuals with a unique set of needs. Breast MRI can be extremely helpful in certain women newly diagnosed with breast cancer. This is especially true in women with dense breasts, women with invasive lobular carcinoma, and in patients with complex standard imaging. If you are newly diagnosed with breast cancer, a good question for your treating physician is, "Do I need a breast MRI. If so, why? If not, why?”
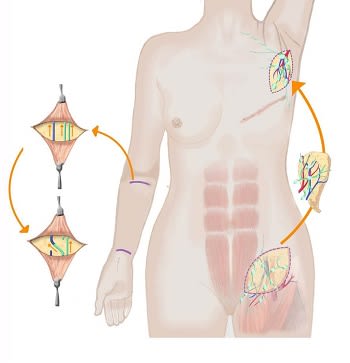
2. Don’t routinely excise all the lymph nodes underneath the arm in patients having partial breast removal (lumpectomy) for breast cancer when only one or two contain cancer.
The guidelines regarding the management of the lymph nodes in women with breast cancer have changed, and once again care should be individualized. This statement is correct, but only if certain conditions are met. In some cases, we do not need to remove the rest of the lymph nodes in a woman in whom only 1 or 2 lymph nodes contained breast cancer. The goal is to avoid creating unnecessary side effects, but we also never want to undertreat cancer.
3. Don’t routinely order specialized tumor gene testing in all new breast cancer patients.
Again, the key word in this sentence is "routinely.” Most importantly, these tests should not be done on patients who are not candidates for chemotherapy or are unwilling to receive chemotherapy. Most of the time, these tests provide selected patients with information about their risk of cancer spreading (metastasizing) at a later date, or their risk of dying from breast cancer in order to estimate the likelihood that they would benefit from chemotherapy. Most of the time, these tests are especially helpful in selected patients with early stage, hormone receptor positive (ER + or PR +) cancers.
4. Don’t routinely re-operate on patients if the cancer is close to the edge of the excised lumpectomy tissue.
This guideline was included to draw attention to the new data that confirms that a minimal rim of normal tissue is all that is needed between the tumor that is removed and the tissue that remains. If surgeons no longer demand wide margins in women with invasive breast cancer, repeat surgeries can be minimized, cosmetic outcome improved, return to normal activities facilitated, and health care costs decreased. However, if cancer cells are found at the edge of the surgically removed tumor, repeat surgery (re-excision) is still an important component of care.
5. Don’t routinely perform a double mastectomy in patients who have a single breast with cancer.
Okay, this guideline is a little trickier. It is important that women newly diagnosed with cancer in one breast understand that removal of the other (“good”) breast does not improve survival. Nevertheless, in certain patients, it does make sense after adequate counseling to perform a double mastectomy. This is when an honest discussion between the patient and her physicians, and careful consideration of all options taking into account the patient’s priorities is critically important in determining the best treatment.
My take-home message is that guidelines help determine the usual best treatment. As always, up-to-date, individualized, compassionate care is the most important component of the art medicine.
More information is available on the Choosing Wisely website and the complete article can be found in the Annals of Surgical Oncology (open access /free).


























































)


)
)
)




