Comprehensive Care For Your Rehabilitation
When you stay at Stamford Hospital’s Van Munching Rehabilitation Unit, our providers take a multidisciplinary, intensive approach to your medical and physical rehabilitation needs. Together with you and your medical team, our therapists create a plan to help you return to an active, healthy lifestyle.
Your doctor may recommend a stay at our acute inpatient rehabilitation facility if you:
Conditions We Treat
Our specialists have extensive training and certification to care for patients with:
- Amputation.
- Brain injury.
- Cardiac or respiratory disease.
- Femur or hip fracture.
- Musculoskeletal (bone, joint, or muscle) disorder.
- Neurological disorders and injuries like Parkinson’s disease and multiple sclerosis.
- Orthopedic and sports injuries.
- Polyarthritis (several painful joints).
- Stroke.
- Traumatic injuries.
- Total joint replacements.
Our Rehab Team Of Experts
During your stay, the following specialists may help you develop and reach your goals.
-
PHYSICIANS
-
PHYSICAL THERAPISTS
-
OCCUPATIONAL THERAPISTS
-
SPEECH-LANGUAGE PATHOLOGIST
-
NURSES
Physiatrist Care During Your Stay
Physiatrists are medical doctors who are specially trained in rehabilitation and physical medicine. During your stay, the Van Munching Unit physiatrists manage your individualized medical treatment and rehabilitation program.
Physical Therapy During Your Stay
As part of the required therapy on the Van Munching Unit, a physical therapist will work with you to increase your balance, strength, and coordination with the goal of maximizing functional mobility and independence while promoting safety.
Some of the tasks you work on with your therapist may include:
- Getting in and out of bed.
- Standing up from a chair.
- Walking and stair training.
- Exercises and activities to improve strength, balance, coordination, and endurance.
Ahead of discharge, physical therapists work with your interdisciplinary team to make recommendations for assistive devices, additional services after discharge, and appropriate next level of care.

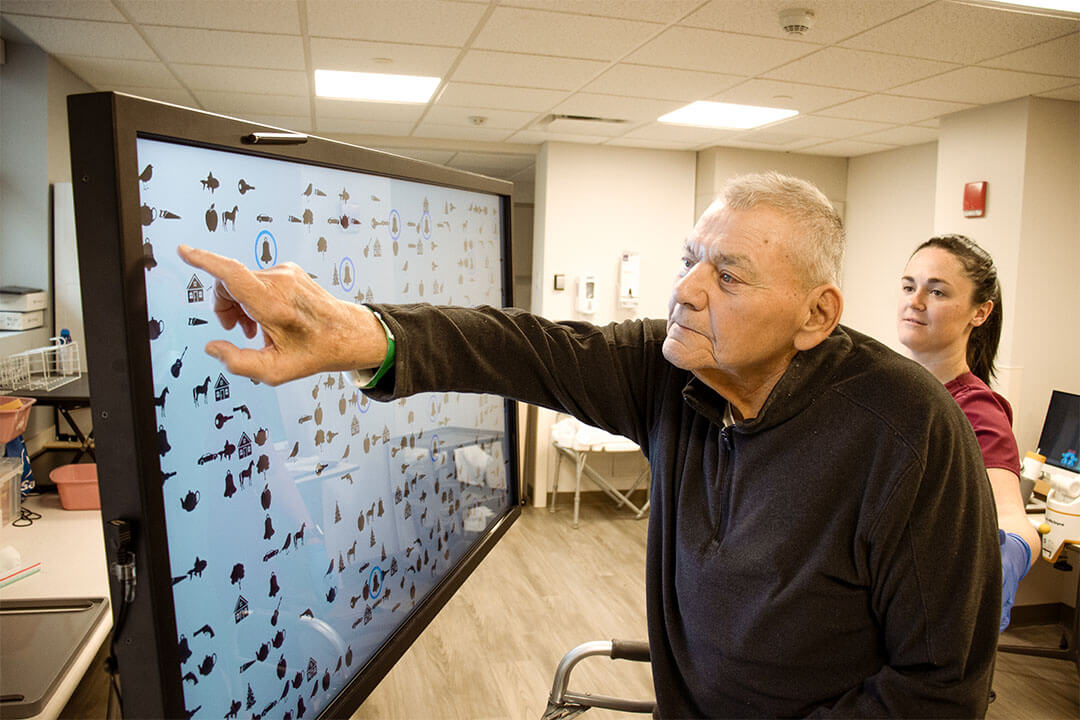
Occupational Therapy During Your Stay
As part of the required therapy on the Van Munching Unit, an occupational therapist will help improve your ability to do daily activities. Your therapist will conduct an assessment and develop a treatment plan based on your cognition, vision, motor planning, and coordination. Our therapists focus on purposeful, goal-directed activities including self-care skills such as bathing, dressing, self-feeding, and toileting, implementing lifestyle modifications as needed.
Ahead of discharge, the therapists will assess the patient’s needs and any barriers. You and your care partners may receive training for the use of adaptive equipment to improve safety and independence.

Speech-Language Care During Your Stay
If needed as part of your therapy on the Van Munching Unit, a speech-language pathologist will help treat problems that affect your ability to swallow, communicate, or think, particularly due to diagnoses including aphasia, apraxia, dysarthria, dysphagia, and cognitive impairment. Our goal is to help patients improve their quality of life before returning home or to the next level of care.
Together with the patient and their care partners, our specialists provide the skills and strategies for the patient to:
- Express their wants and needs.
- Engage socially.
- Solve problems in order to complete household, community, and work-related tasks.
- Eat and drink safely.

Rehab Nurses During Your Stay
Registered nurses on the Van Munching Unit have specialty training to provide 24/7 monitoring and direct care. They also support rehabilitation self-care strategies and educate patients in health care management. Our care goes beyond nursing with an interdisciplinary approach that includes working closely with patients, their families, physicians, therapists, aides, and social workers.
In addition, Van Munching Unit nurses also:
- Specialize in assisting patients affected by chronic illness and disability through health restoration, maintenance, and promotion.
- Function as care coordinators, providing medication, diabetes, nutrition, and stroke education during the patient’s stay.
- Serve as patient advocates and provide input into the effectiveness of the treatment plan on an ongoing basis.

Consulting Services Available
When you stay on the Van Munching Unit, you may receive services from the following members of our team.Hear From Our Patients
Acute Inpatient Rehab Facility FAQs
-
What should you bring to VMU?
Comfortable leisure clothing or sweatsuits and closed-toed shoes or sneakers are recommended.
Please bring pajamas, underwear, and a sweater or coat.
Basic toiletries are provided; however, you may prefer to bring your own deodorant, shampoo/conditioner, toothpaste, hairbrush, and lotion.
Please bring at least five days’ worth of clothing.
We recognize the role that technology plays in our daily lives. The use of a cell phone, iPad, or laptop computer is allowed and is the responsibility of the patient. Please bring chargers for your personal electronics.
VMU has a lending library, but feel free to bring your own reading materials.
-
What shouldn’t you bring to VMU?Slip on/open-back shoes or heeled shoes are not recommended.
Please do not bring any electrical equipment such as a hair dryer or curling iron.
Do not bring any jewelry, credit cards, and large sums of money or any other valuables.
-
What is a typical day like on the inpatient rehab floor?On the first day of therapy, patients are evaluated by physical therapy, occupational therapy, and speech therapy (as appropriate). The therapist will educate patients regarding their evaluations, spend time planning appropriate goals with the patients, and discuss expectations for safe, appropriate discharge plans. Patients should actively participate in setting goals.
Each patient receives 3 hours of individualized therapy Monday- Friday. There is modified weekend programming.
-
Are visitors allowed at Van Munching?Family and friends are an important part of the rehabilitation process. They are welcome every day.
Family members or care partners may be asked to attend treatment sessions for training to learn techniques to improve the patient’s safety when they return home.
Children must be accompanied by a supervising adult and be in good health.
-
How will you know the therapy schedule or discharge plan?A whiteboard with information regarding your therapy schedule and other pertinent information will be displayed in your room. Your therapy schedule will be updated daily by 4:30 p.m. the day prior.
Planning for discharge begins on the first day of your admission to the Rehabilitation Unit. Typically, the goal is to return patients’ home, with home care therapy or outpatient t herapy. Within a week of your admission, your team will meet to discuss your goals for rehabilitation and develop a plan for your inpatient rehabilitation stay and discharge.










