Addressing the Confusion about Mammograms
Published: October 30, 2015l
By David Gruen, Director, MD, MBA, Women's Imaging and Co-Director of the Breast Center
The American Cancer Society (ACS) issued mammography guidelines this week, adding to the confusion that some women already face when making health decisions. In recommending that average-risk women wait until age 45 to start having annual mammograms, and every other year after age 55, the ACS has begged the question, “Now what?” As breast health experts, these varying guidelines concern us greatly, and should concern women as well. We strongly disagree with the idea that finding breast cancer before age 45 or after age 55 is less important.
We join with the American College of Radiology, the National Comprehensive Cancer Network, The Society of Breast Imaging, and many other health care institutions to strongly encourage women to not change what they are doing. Women at average risk should start annual screening mammography at age 40, and continue every year, for as long as they are healthy. Women at increased risk- either from personal or family history- should talk with their health care provider or a breast health expert about an optimal, personalized screening and risk-reduction program.
The rationale for the ACS’s new guidelines is based on the potential anxiety caused from ‘false positive’ mammography; and the theoretical concepts of over-diagnosis and overtreatment.
The truth is that for every 1000 women who have a screening mammogram, roughly 20 of them (1.9%) will require a biopsy. Of those, six will have breast cancer. In other words, more than 90% of women screened will not require a biopsy to be told they do not have breast cancer. We think those are pretty good odds. And, though recalls from screening may cause some inconvenience and anxiety, we believe this is better than finding out that your late stage breast cancer is incurable.
There is a trend to use terms like, “over-diagnosis” and”over-treatment” by some to reduce necessary screening. The theory is that screening for breast cancer leads to the detection of cancers that would never become significant or cause a woman harm. It has been stated that thousands of breast cancers every year would disappear on their own if left alone. Our stance on the above argument is this: there has never been one proven case of an invasive breast cancer resolving on its own.
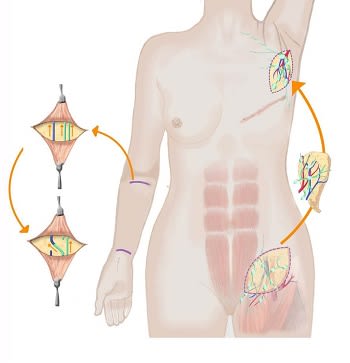
In addition, there is confusion between ductal carcinoma in situ (DCIS) with invasive breast cancer. DCIS constitutes a spectrum of breast lesions, about whose biology we still have much to learn. Some DCIS may, and some will not progress to invasive cancer. Unfortunately, DCIS and invasive breast cancer do not have a blood or other diagnostic test that can distinguish those lesions that may be harmless from those that may be aggressive and potentially deadly. This type of identification still requires detection, best done with mammography, a biopsy, and microscopic analysis.
Connecticut has the highest incidence of breast cancer in the country. According to ACS, about 231,840 new cases of invasive breast cancer will be diagnosed in women this year, and about 40,290 women will die from the disease. In Connecticut they estimate 3,190 residents will be diagnosed with breast cancer this year, and 460 will die from it. There is no magical difference between age 40, 45, or 50 when it comes to breast cancer. As breast care physicians, we see women diagnosed with breast cancer in their 20’s, 30’s, and at every age thereafter.
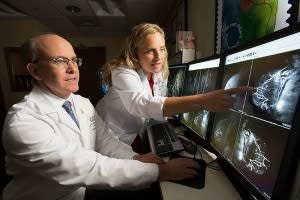
In Stamford, our Women’s Breast Center was the first in the region to offer digital breast tomosynthesis, or 3D mammograms to all women, and we will continue to do so. This breast imaging technology provides significantly more detailed information than traditional mammography. In fact, it has decreased our false positives rate by more than 40% since its introduction, and has improved our cancer detection rate by more than 50%.
We don’t think it’s fair to assume that a woman would prefer not to be screened because it may make her anxious, or because she might need a few extra images to either find, or exclude, a breast cancer. The other option- not being screened regularly- results in a higher likelihood of being diagnosed with later-stage, less curable breast cancer. To us, this is an obvious life-altering choice.
While we still recognize and support the ACS as an important member of the cancer care community, we professionally disagree with these new guidelines. We want to help clarify the facts about mammograms, which no one disputes, including the American Cancer Society:
- Mammography saves lives. The death rate (mortality) for breast cancer has decreased by nearly a third since screening became widespread.
- One in six breast cancers occur in women aged 40-49.
- 40% of ALL THE YEARS OF LIVES SAVED BY MAMMOGRAPHY are for women in their 40’s.
- Between 2010-2014, about 10 percent of the breast cancers diagnosed in our Women’s Breast Center were in women under the age of 45.
- Skipping a yearly mammogram may result in up to 30% of breast cancers going undetected.
You can learn more about our approach to screening as well as the diagnoses and treatment of breast cancer on our Breast Center page.
Featured Expert/ Author


?h=333&iar=0&w=500)





























































)
)
)




