New Targeted Treatment With Intravesical Therapy for High-Risk Bladder Cancer
Published: October 20, 2025l
A new level of person-centered care is available at Stamford Health’s Carl & Dorothy Bennett Cancer Center (BCC) with the arrival of intravesical therapy, an innovative treatment for patients with high-risk, non-muscle invasive bladder cancer (NMIBC). Intravesical therapy involves placing medications such as chemotherapy and immunotherapy directly into the bladder. The localized, targeted approach has fewer side effects than systemic chemotherapy and significantly reduces the recurrence rate of these common and serious cancers compared to surgery alone.
“Intravesical therapy is the preferred treatment for patients with high-risk NMIBC including stage Ta, stage T1, and carcinoma in situ (CIS), cancers that are confined to the bladder lining and have a high-risk of recurrence and progression,” explained Dr. Hugh Lavery, chief of the division of urology at Stamford Health. “For these patients, our treatment goals are to prevent recurrence and progression to the bladder muscle, which would give it (the cancer) the capacity to metastasize throughout the body.”
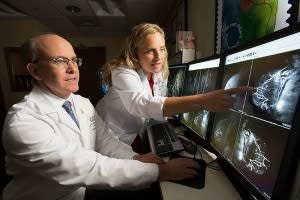
For years, the standard of care treatment for high-risk NMIBC involved surgery to remove the tumor (called a transurethral resection of bladder tumor, or TURBT), followed by intravesical treatment with a type of immunotherapy called bacillus Calmette-Guérin (BCG). In recent years, a shortage of BCG spurred the intravesical use of a combination of chemotherapy drugs, gemcitabine and docetaxel, which proved to be as effective as BCG in fighting the cancer and has a lower risk of complications. In December 2024, Dr. Lavery and Dr. Anthony Gulati, a medical oncologist at Stamford Health, spearheaded the intravesical therapy program at the BCC, where a multidisciplinary team of specialists, including medical oncologists, surgical oncologists, radiation oncologists, pathologists, and oncology nurses closely collaborate to ensure the accurate diagnosis, staging, and treatment of a wide range of cancers.
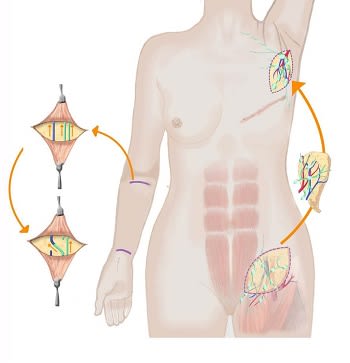
In intravesical therapy, medication is directly inserted into the patient’s bladder through a urinary catheter. The medication remains in the bladder for several hours, after which it is either voided by the patient or drained from the bladder via the catheter. The therapy is typically given in a single dose to a patient with NMIBC shortly after a TURBT. A few weeks after surgery, if the findings on the pathology report show high-risk cancer, the patient will undergo an induction course of six weekly intravesical therapy cycles, followed by a monthly maintenance course for 18 months. Throughout the maintenance course, patients are monitored every three months with cystoscopy and urinary cytology to detect cancer recurrence.
“Intravesical therapy has been a game changer for patients with high-risk NMBIC,” said Dr. Lavery. “It is quite successful at preventing tumor progression. Many people are cured from the initial TURBT and induction course of gemcitabine and docetaxel alone.”
“Before the intravesical therapy program, patients relied solely on surgery for treatment or they were referred out of the health system,” added Lusine Santa, a nurse and the oncology service line manager at the BCC and a key organizer of the intravesical therapy program. “By offering intravesical therapy to patients, we can help reduce recurrence rates and delay progression, leading to fewer repeat surgeries and hospitalizations. Additionally, successful intravesical therapy helps patients keep their bladders instead of undergoing a major operation such as radical cystectomy, which greatly improves outcomes and quality of life.”
“Intravesical therapy is a great option for people who cannot or do not want to have major abdominal bladder surgery,” said Dr. Lavery. “NMIBC mainly affects older adults, many who are not fit or are unwilling to have surgery at this stage of their lives.”
“The BCC is an ideal setting for patients undergoing intravesical therapy who must wait several hours before they can void the therapy,” he added. “One of my patients, a 60-year-old woman, told me it was a pleasure to go to the BCC for her therapy, because she can enjoy amenities such as music therapy, massage, and counseling. These person-centered services have greatly enhanced patient satisfaction and the overall patient experience.”
“Intravesical therapy is the preferred treatment for patients with high-risk NMIBC including stage Ta, stage T1, and carcinoma in situ (CIS), cancers that are confined to the bladder lining and have a high-risk of recurrence and progression,” explained Dr. Hugh Lavery, chief of the division of urology at Stamford Health. “For these patients, our treatment goals are to prevent recurrence and progression to the bladder muscle, which would give it (the cancer) the capacity to metastasize throughout the body.”
For years, the standard of care treatment for high-risk NMIBC involved surgery to remove the tumor (called a transurethral resection of bladder tumor, or TURBT), followed by intravesical treatment with a type of immunotherapy called bacillus Calmette-Guérin (BCG). In recent years, a shortage of BCG spurred the intravesical use of a combination of chemotherapy drugs, gemcitabine and docetaxel, which proved to be as effective as BCG in fighting the cancer and has a lower risk of complications. In December 2024, Dr. Lavery and Dr. Anthony Gulati, a medical oncologist at Stamford Health, spearheaded the intravesical therapy program at the BCC, where a multidisciplinary team of specialists, including medical oncologists, surgical oncologists, radiation oncologists, pathologists, and oncology nurses closely collaborate to ensure the accurate diagnosis, staging, and treatment of a wide range of cancers.
In intravesical therapy, medication is directly inserted into the patient’s bladder through a urinary catheter. The medication remains in the bladder for several hours, after which it is either voided by the patient or drained from the bladder via the catheter. The therapy is typically given in a single dose to a patient with NMIBC shortly after a TURBT. A few weeks after surgery, if the findings on the pathology report show high-risk cancer, the patient will undergo an induction course of six weekly intravesical therapy cycles, followed by a monthly maintenance course for 18 months. Throughout the maintenance course, patients are monitored every three months with cystoscopy and urinary cytology to detect cancer recurrence.
“Intravesical therapy has been a game changer for patients with high-risk NMBIC,” said Dr. Lavery. “It is quite successful at preventing tumor progression. Many people are cured from the initial TURBT and induction course of gemcitabine and docetaxel alone.”
“Before the intravesical therapy program, patients relied solely on surgery for treatment or they were referred out of the health system,” added Lusine Santa, a nurse and the oncology service line manager at the BCC and a key organizer of the intravesical therapy program. “By offering intravesical therapy to patients, we can help reduce recurrence rates and delay progression, leading to fewer repeat surgeries and hospitalizations. Additionally, successful intravesical therapy helps patients keep their bladders instead of undergoing a major operation such as radical cystectomy, which greatly improves outcomes and quality of life.”
“Intravesical therapy is a great option for people who cannot or do not want to have major abdominal bladder surgery,” said Dr. Lavery. “NMIBC mainly affects older adults, many who are not fit or are unwilling to have surgery at this stage of their lives.”
“The BCC is an ideal setting for patients undergoing intravesical therapy who must wait several hours before they can void the therapy,” he added. “One of my patients, a 60-year-old woman, told me it was a pleasure to go to the BCC for her therapy, because she can enjoy amenities such as music therapy, massage, and counseling. These person-centered services have greatly enhanced patient satisfaction and the overall patient experience.”
Featured Expert/ Author

Stamford Health Medical Group Member





























































)


)
)
)




