How to Distribute COVID-19 Vaccines
Published: September 04, 2020l
This article was first published in The Hill. Republished with permission. The views expressed by contributors are their own and not the view of The Hill.
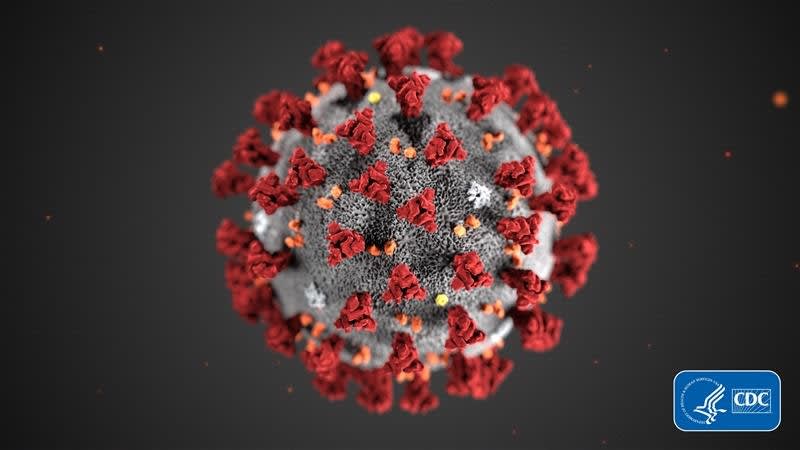
The development of new COVID vaccines is unleashing hope across the nation that we will soon gain control of this terrible pandemic. But vaccine discovery is only the beginning. Vaccinating 330 million Americans will be a tremendous operational undertaking.
The surprising urgency and ferocity of the pandemic created a disjointed and inefficient approach this Spring. This time we can do better, but I worry.

Delays delivering innovation to the masses is common in history. Thomas Edison invented incandescent lightbulbs in 1879. But it was not until 1925 that half of American homes had electric power to light them. What was needed was a pathway to deliver this innovation to the public on a broad scale: wiring, light switches, electric meters, and more.
Success in delivering this innovation faces many hurdles. But three common sense things, grounded in decisive action — using resources that the federal, state and local governments already have in place — will make this possible.
First, we need clear accountability. We need a decision about who is writing the roadmap for vaccine distribution. Right now, that is unclear.
For decades, the Advisory Committee on Immunization Practice (ACIP) has made recommendations to the Centers for Disease Control and Prevention (CDC) on vaccine policy. This leadership role was clearly and effectively demonstrated during the 2009 H1N1 pandemic. The ACIP already has a working group for COVID-19.
Despite this, on July 21st, the National Institutes of Health and the CDC asked the National Academies of Sciences, Engineering, and Medicine, and the National Academy of Medicine to launch a committee to plan for the allocation of COVID-19 vaccines.
In addition to this confusion, there is Operation Warp Speed (OWS). Among other things, it has been assigned responsibility for COVID-19 vaccines. OWS indicates that the Department of Defense will also have some role.
Whichever entity is placed in charge will have to determine the complex and multi-stage pathway that will bring vaccines from production sites to the public. The biggest mistake the government could make would be to try to design this from scratch.
The federal government, under the CDC’s leadership, has facilitated both public and private infrastructure to deliver life-saving vaccines in the past successfully. All states maintain pandemic influenza plans. According to the Association of Immunization Managers and three other public health associations, a pathway would best be constructed by building upon existing plans.
For example, the Vaccines for Children program was established in 1994 to provide vaccines to Medicaid-eligible and uninsured children. State immunization officials manage the program to enroll public and private providers, receive and approve vaccine orders, document doses administered, and manage vaccine supply and inventory. The program, managed by the CDC, is highly effective and has provided vaccines to 40 million children.
During the 2009 H1N1 pandemic, this system was expanded to enroll adults. State and local health officials, along with the American Medical Association, identified providers including obstetricians, gynecologists, and other physicians who treat and immunize adults. Altogether, the program distributed approximately 138 million doses of the H1N1 vaccine.
Second, we need clear rules of the road. In this case, we need to make the difficult decisions about who will get the vaccine once doses become available.
Should we start with essential workers? How about those most at-risk medically? Do we prioritize those populations who have been most affected? Our strategy needs to be guided by the principles of saving lives and getting back to normal quickly, and by science, not special interests.
Lastly, we need a robust communication plan. A poll by the Pew Research Center in May found that 27 percent of those asked said they would not get a COVID-19 vaccine if it were available today. We will need to convince even the most skeptical of Americans that the vaccine is safe and effective if we are going to achieve herd immunity.
Moreover, we need to communicate the importance of vaccination to those populations that are the hardest to reach, because they can often be the most vulnerable. For these groups, it’s about being on the ground and in the community. These groups were among the hardest hit by the pandemic, and we may need to restore their trust in the public health system.
Distributing this vaccine in a timely fashion to all Americans is doable. We do it every year for the flu vaccine, and we did it during the 2009 H1N1 pandemic. But we must begin planning to avoid false starts, confusion and delays. It’s time to get moving.
Featured Expert/ Author