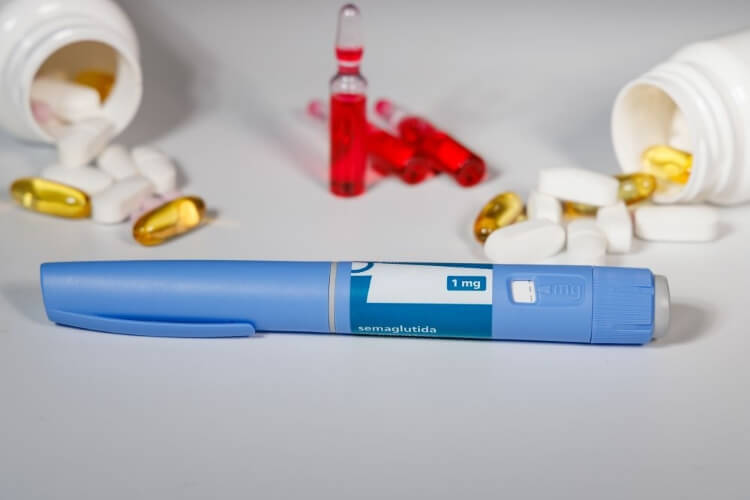
It’s no secret that GLP-1 medications (a class of drugs used to treat Type 2 diabetes, weight management, cardiovascular risk reduction, and obstructive sleep apnea) can help people dealing with obesity and its comorbidities shed weight effectively, but what happens when they stop? A meta-analysis from Stamford Health found that patients are likely to gain the pounds back within a few months if they stop the injections. The findings reinforce the notion that obesity is a chronic disease with the need for continuous medication to manage it.
Obesity, defined as having a body mass index (BMI) of 30 or higher, affects nearly 40% of Americans, and nearly 75% of Americans are overweight, or have a BMI of 25.5 to 30. It is one of the most prevalent chronic illnesses in the United States and increases the risk of conditions for nearly every part of the body. Successfully managing obesity requires a mixture of lifestyle modifications and medication. Since their introduction into the market 20 years ago, GLP-1 injections have been the most successful at controlling the complex forces inside the body that regulate weight.
Stamford Health’s Executive Director of Research, Suzanne Rose, PhD, partnered with Sacred Heart Health physician assistant students to determine what happens when patients stop the treatment of their chronic condition. They reviewed hundreds of different studies to track 2,372 participants who were prescribed both GLP-1 medication and lifestyle modifications such as nutrition counseling and exercise.
“On average, they gained about 60% of the weight back within a few months to a year – despite those lifestyle modifications,” said Rose. “That can be a devastating thing for the patient to deal with.”
Rose noted that many people don’t stop the medication because it’s working or they reach a goal weight; they quit due to side effects common with the injectables (such as nausea or diarrhea), dislike of giving themselves daily shots, or the prohibitive cost, especially if insurance doesn’t cover the medication.
“Obesity is a chronic disease so we should treat it the same way as, say, high blood pressure, where you just take those drugs every single day for the rest of your life,” said Rose. “So many people try so hard to lose weight, and these drugs help them do that.”
And it’s not just excess weight that reappears. Obesity is linked to countless other chronic conditions and diseases including heart disease, diabetes, stroke, some cancers, and sleep apnea. When a person regains weight that they previously lost, they also regain the health risks that are associated with them. “The forces inside the body are so strong that it’s important for patients to understand that these current medications are meant for long-term use ,” said Dr. Maria Cecilia Asnis, Medical Director of the Center for Weight Management at Stamford Health.
As with most life-long decisions, clear expectations, including the positives and negatives, should be discussed from the beginning. “I am upfront with all of my patients that it’s a big deal to go on the medications for potentially the rest of your life,” Asnis said. “I know from practicing for more than 10 years that when people stop – even if their lifestyle modifications such as diet and exercise are perfect – there will almost always be weight regain. That’s because we’re no longer addressing what’s going on inside of the body.”
If we stop treating weight issues, we increase the risk for countless other conditions. “Weight touches everything,” said Asnis. “It really is the root cause of so many issues from cardiovascular to endocrinological, fertility, joints, cancer, everything.”
While at first glance the findings of Rose’s meta-analysis may seem shocking, the intent is to reinforce the idea of the benefits of these drugs as treatment to the most common chronic condition in the United States.
“The bottom line of our paper is thinking about this class of drugs as long-term therapy and the reasons for going off of them,” said Rose. “And if a patient wants to stay on them and is experiencing side effects, what can we do to help them.”
If you’re interested in losing weight and unsure of where to start, please contact Center For Weight Management at Stamford Health for a consultation.
Obesity, defined as having a body mass index (BMI) of 30 or higher, affects nearly 40% of Americans, and nearly 75% of Americans are overweight, or have a BMI of 25.5 to 30. It is one of the most prevalent chronic illnesses in the United States and increases the risk of conditions for nearly every part of the body. Successfully managing obesity requires a mixture of lifestyle modifications and medication. Since their introduction into the market 20 years ago, GLP-1 injections have been the most successful at controlling the complex forces inside the body that regulate weight.
Stamford Health’s Executive Director of Research, Suzanne Rose, PhD, partnered with Sacred Heart Health physician assistant students to determine what happens when patients stop the treatment of their chronic condition. They reviewed hundreds of different studies to track 2,372 participants who were prescribed both GLP-1 medication and lifestyle modifications such as nutrition counseling and exercise.
“On average, they gained about 60% of the weight back within a few months to a year – despite those lifestyle modifications,” said Rose. “That can be a devastating thing for the patient to deal with.”
Rose noted that many people don’t stop the medication because it’s working or they reach a goal weight; they quit due to side effects common with the injectables (such as nausea or diarrhea), dislike of giving themselves daily shots, or the prohibitive cost, especially if insurance doesn’t cover the medication.
“Obesity is a chronic disease so we should treat it the same way as, say, high blood pressure, where you just take those drugs every single day for the rest of your life,” said Rose. “So many people try so hard to lose weight, and these drugs help them do that.”
And it’s not just excess weight that reappears. Obesity is linked to countless other chronic conditions and diseases including heart disease, diabetes, stroke, some cancers, and sleep apnea. When a person regains weight that they previously lost, they also regain the health risks that are associated with them. “The forces inside the body are so strong that it’s important for patients to understand that these current medications are meant for long-term use ,” said Dr. Maria Cecilia Asnis, Medical Director of the Center for Weight Management at Stamford Health.
As with most life-long decisions, clear expectations, including the positives and negatives, should be discussed from the beginning. “I am upfront with all of my patients that it’s a big deal to go on the medications for potentially the rest of your life,” Asnis said. “I know from practicing for more than 10 years that when people stop – even if their lifestyle modifications such as diet and exercise are perfect – there will almost always be weight regain. That’s because we’re no longer addressing what’s going on inside of the body.”
If we stop treating weight issues, we increase the risk for countless other conditions. “Weight touches everything,” said Asnis. “It really is the root cause of so many issues from cardiovascular to endocrinological, fertility, joints, cancer, everything.”
While at first glance the findings of Rose’s meta-analysis may seem shocking, the intent is to reinforce the idea of the benefits of these drugs as treatment to the most common chronic condition in the United States.
“The bottom line of our paper is thinking about this class of drugs as long-term therapy and the reasons for going off of them,” said Rose. “And if a patient wants to stay on them and is experiencing side effects, what can we do to help them.”
If you’re interested in losing weight and unsure of where to start, please contact Center For Weight Management at Stamford Health for a consultation.
Featured Expert/ Author