By Corinne VanBeek, MD


Tell us a little about yourself: What made you want to become an orthopedic surgeon?
As much as I would love to tell a grandiose story reflecting my decision to enter medicine, I was simply quite practical and chose the field with the greatest potential to fulfill my career desires. Medicine promised to consistently challenge me in a variety of ways and offered unparalleled satisfaction and endless opportunities; the latter becomes very important to restless souls like me who quickly get bored with monotony. The diversity in medicine enabled me to choose a field (orthopedic surgery) in which my time is shared between the office (diagnosing and treating patients), the operating room (restoring anatomy and function and being technically challenged), and the virtual classroom (mentoring and teaching).What drew you to the shoulder and elbow, specifically?
During my orthopedic training, I developed a passion for shoulder and elbow surgery. I see patients of all ages and lifestyles, from teenagers aspiring to be the next MLB pitcher to octogenarians wanting to improve their golf game. I treat a variety of conditions, from trauma and fractures around the shoulder and elbow to rotator cuff disorders and arthritis.....and everything in between! Treatments for these problems range from nonoperative management to surgical interventions involving open and arthroscopic approaches. Surgical techniques are constantly evolving to improve outcomes in these areas.What have your patients taught you during your time at Stamford Health?
Caring for people is a unique privilege. I am constantly reminded that no two patients are the same, and I must listen to each patient. Communication is at the forefront to providing excellent patient care.What is the most common problem you see in your patients?
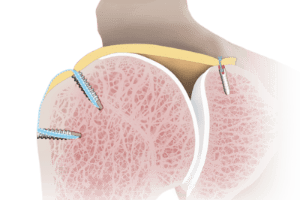
The most common shoulder and elbow problems I see are related to the rotator cuff, or the group of muscles and tendons around the shoulder joint. This ranges from tendonitis without discrete tears to large and massive rotator cuff tears.How has recently joining the HSS Orthopedics at Stamford Health collaborative made a difference in the trajectory of your career and in patient care?
The partnership between Hospital for Special Surgery (HSS) and Stamford Health promotes quality care at all levels. We routinely critically analyze every point of care and treatment to perfect our patients' experiences and outcomes. The partnership promotes education of all caregivers, including nurses, physical therapists, doctors and patients alike with conferences and outreach lectures. Through education and quality care, we are able to consistently offer the latest and best techniques with a low complication rate.Hearing the phrase, “You may need a new shoulder” can be frightening for a patient. In fact, some put off this type of surgery for months, even years. What are your thoughts on advising patients on exploring all non-surgical options before embarking on total or partial replacement surgery?
The truth is no one ever wants surgery unless it is necessary. A shoulder replacement is an elective surgery. Our primary goal is to improve a patient's quality of life and symptoms without surgery, until the only remaining option is surgery. I frequently tell my patients they will know when they need the surgery. At a certain point, symptoms may become intolerable and the condition severe enough to warrant surgery. Fortunately, we have an excellent reliable surgery (shoulder replacement surgery) to restore their function and greatly improve their quality of life when they are ready to entrust us with their care.What is one recent advancement in your field that is innovative or integral to your work?
The greatest advancement in shoulder surgery over the past few decades was the introduction of arthroscopy, or minimally invasive joint surgery. Shoulder surgery has undergone a paradigm shift over the past 20 to 30 years, with fewer open (big incision) surgical procedures being performed and more arthroscopic techniques being developed. We have refined our arthroscopic instrumentation and techniques over the past 20 years or so to improve outcomes. A more recent advancement in shoulder surgery is orthobiologics, or using the body's natural substances to help an injury heal faster. We are in the phase of investigating their effectiveness, including PRP (platelet rich plasma), patches, and stem cells, and tracking outcomes with their use.About The Author
Dr. VanBeek is a shoulder and elbow specialist with expertise in shoulder repair and reconstruction, including minimally invasive techniques as well as traditional and reverse shoulder replacements. View her complete profile.Featured Expert/ Author