By Corinne VanBeek, MD
Every MLB fan, Mets and Yankees fans alike, has heard the words "Tommy John" repetitively over the past year or so....and not in a good way. ESPN.com is naming it an epidemic. What is ailing our great baseball pitchers and what do our youth pitchers need to know to prevent "Tommy John" injuries?
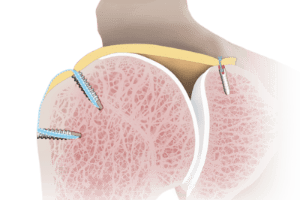
Let's start with the basics. The elbow joint is where the arm bone (humerus) meets the two forearm bones (the radius and ulna). It is a hinge and pivot joint, meaning it bends, straightens, twists, and rotates. On the inner and outer aspects of the elbow, the collateral ligaments hold the joint together. Ligaments are tough yet flexible tissues that connect two bones and hold joints together. The ligament on the inner aspect of the elbow is the ulnar collateral ligament (UCL).
Injury to the UCL is common among overhead-throwing athletes, especially baseball pitchers, as the ligament must withstand extreme stresses as it stabilizes the elbow during the forceful overhead throw. In 1974, Dr. Jobe performed the first reconstruction of the UCL in baseball great Tommy John, for whom the surgery was subsequently named. Reconstruction entails recreating the ligament with a tendon, versus a repair that brings the two ends of the torn ligament back together.
The incidence of UCL injuries has escalated over the past few years, with estimates that one in three professional baseball pitchers has had a UCL reconstruction. Why? Repetitive overhead throwing consistently stresses the ligament and creates microtrauma in the ligament and degeneration over time. As the ligament degenerates, it no longer functions as well to hold the elbow joint together and consequently causes pain and laxity (looseness) at the elbow. Most UCL injuries are overuse injuries from an ongoing, degenerative process that thins the ligament out until one final throw when the ligament ruptures off the bone.
UCL injury rates have increased seven to tenfold in the last ten years. Over half of professional baseball players had a precipitating minor injury to the UCL when playing youth baseball. The injury progresses over years of playing and then as a young MLB player, they experience the final blow that necessitates "Tommy John" surgery.
Why are our youth at risk? Our youth are playing too much and too hard and are overusing their elbows (and shoulders). Frequently, they are playing year round baseball and pitching too much in a game and in a week. Pitch counts have been established as guides to the number of pitches a young pitcher should maximally throw per game depending on age. While the pitch counts may be observed during their school games, the players are playing in multiple leagues and playing pick up baseball. Furthermore, they are not getting enough rest and are playing while fatigued. A pitcher who is fatigued has a 36 times greater risk of sustaining a shoulder or elbow injury....and that injury may necessitate surgery. Sport specialization has also become a problem. Our youth are focusing on a single sport and within that sport, one position (ie: pitcher). The same muscles and ligaments (and growth plates in growing athletes) are constantly being stressed.
The goal for our youth should be focused on prevention. However, once an injury does occur, it is important to be evaluated by an orthopaedic surgeon. Pain at the inner elbow may be the first sign, especially when it develops during certain phases of throwing. Injuries to the ligament vary from irritation of the ligament to complete rupture. Management of the injury depends on its severity. An MRI (magnetic resonance imaging) may be obtained to further evaluate the integrity of the ligament and associated pathology. Sometimes surgery is warranted when severe injury to the ligament has occurred. The first line of nonoperative treatment entails rest of the ligament with no throwing at all for a certain duration of time. Physical therapy when indicated focuses on regaining elbow motion, strength, and neuromuscular control. Frequently there are predisposing factors, such as poor pitching mechanics, shoulder weakness and motion deficits, or core and lower extremity weakness. All of these factors need to be evaluated and addressed to prevent injury progression or recurrent injury. No matter what the treatment plan, it will take a team of providers, including coaches, parents, physical therapists, athletic trainers, and orthopaedists, to return the athlete to play and prevent reinjury.
Every MLB fan, Mets and Yankees fans alike, has heard the words "Tommy John" repetitively over the past year or so....and not in a good way. ESPN.com is naming it an epidemic. What is ailing our great baseball pitchers and what do our youth pitchers need to know to prevent "Tommy John" injuries?
Let's start with the basics. The elbow joint is where the arm bone (humerus) meets the two forearm bones (the radius and ulna). It is a hinge and pivot joint, meaning it bends, straightens, twists, and rotates. On the inner and outer aspects of the elbow, the collateral ligaments hold the joint together. Ligaments are tough yet flexible tissues that connect two bones and hold joints together. The ligament on the inner aspect of the elbow is the ulnar collateral ligament (UCL).
Injury to the UCL is common among overhead-throwing athletes, especially baseball pitchers, as the ligament must withstand extreme stresses as it stabilizes the elbow during the forceful overhead throw. In 1974, Dr. Jobe performed the first reconstruction of the UCL in baseball great Tommy John, for whom the surgery was subsequently named. Reconstruction entails recreating the ligament with a tendon, versus a repair that brings the two ends of the torn ligament back together.
The incidence of UCL injuries has escalated over the past few years, with estimates that one in three professional baseball pitchers has had a UCL reconstruction. Why? Repetitive overhead throwing consistently stresses the ligament and creates microtrauma in the ligament and degeneration over time. As the ligament degenerates, it no longer functions as well to hold the elbow joint together and consequently causes pain and laxity (looseness) at the elbow. Most UCL injuries are overuse injuries from an ongoing, degenerative process that thins the ligament out until one final throw when the ligament ruptures off the bone.
UCL injury rates have increased seven to tenfold in the last ten years. Over half of professional baseball players had a precipitating minor injury to the UCL when playing youth baseball. The injury progresses over years of playing and then as a young MLB player, they experience the final blow that necessitates "Tommy John" surgery.
Why are our youth at risk? Our youth are playing too much and too hard and are overusing their elbows (and shoulders). Frequently, they are playing year round baseball and pitching too much in a game and in a week. Pitch counts have been established as guides to the number of pitches a young pitcher should maximally throw per game depending on age. While the pitch counts may be observed during their school games, the players are playing in multiple leagues and playing pick up baseball. Furthermore, they are not getting enough rest and are playing while fatigued. A pitcher who is fatigued has a 36 times greater risk of sustaining a shoulder or elbow injury....and that injury may necessitate surgery. Sport specialization has also become a problem. Our youth are focusing on a single sport and within that sport, one position (ie: pitcher). The same muscles and ligaments (and growth plates in growing athletes) are constantly being stressed.
The goal for our youth should be focused on prevention. However, once an injury does occur, it is important to be evaluated by an orthopaedic surgeon. Pain at the inner elbow may be the first sign, especially when it develops during certain phases of throwing. Injuries to the ligament vary from irritation of the ligament to complete rupture. Management of the injury depends on its severity. An MRI (magnetic resonance imaging) may be obtained to further evaluate the integrity of the ligament and associated pathology. Sometimes surgery is warranted when severe injury to the ligament has occurred. The first line of nonoperative treatment entails rest of the ligament with no throwing at all for a certain duration of time. Physical therapy when indicated focuses on regaining elbow motion, strength, and neuromuscular control. Frequently there are predisposing factors, such as poor pitching mechanics, shoulder weakness and motion deficits, or core and lower extremity weakness. All of these factors need to be evaluated and addressed to prevent injury progression or recurrent injury. No matter what the treatment plan, it will take a team of providers, including coaches, parents, physical therapists, athletic trainers, and orthopaedists, to return the athlete to play and prevent reinjury.
Featured Expert/ Author